An Accidental Finding of Brugada Pattern in an Asymptomatic Woman: A Case Report
Authors : Meher Alam. MD, Jaskaran Purewal. MD, Pramod Bhattarai. MD, George Yatzkan. MD, Odalys Frontela. MD
Introduction:
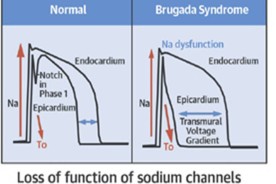
- Brugada syndrome is defined by pseudo-right bundle branch block and persistent ST elevation in leads V1 and V2 along with clinical symptoms2.
- The arrhythmic mechanism of Brugada syndrome likely originates from the connexome; a network of coordinated proteins found at the intercalated disks4.
- It is one of the leading causes of sudden cardiac death in an apparently normal heart. Contributing factors include family history of sudden deaths in one or more relatives or atrial fibrillation6.
- Men with previous ventricular arrythmias.
- Patients who present with the pseudo-right bundle branch and ST elevation in leads V1 and V2 but remain asymptomatic without meeting other clinical criteria are said to have the Brugada pattern5.

Case Description (cont.):
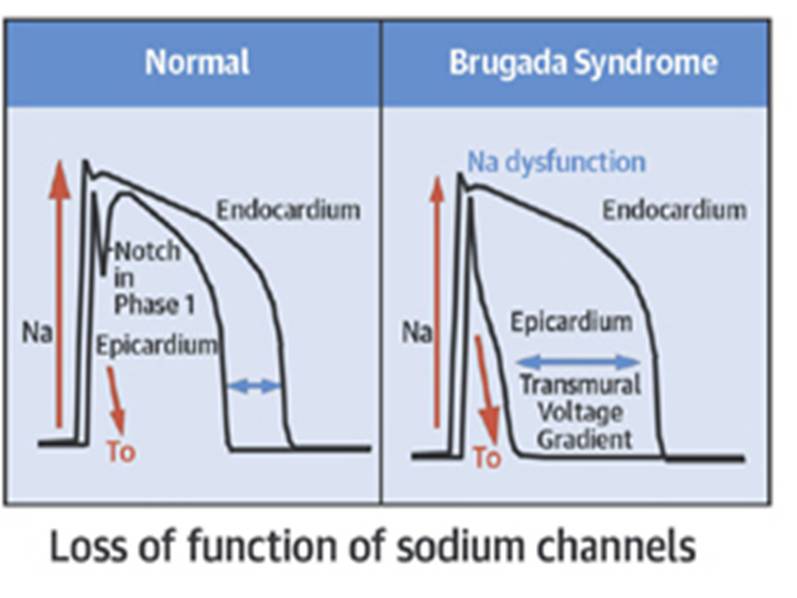
A 52-year-old female with a history of hypertension (controlled) was admitted to the hospital with complaints of dry cough and malaise. She was worked up for upper respiratory disease, not excluding viral pneumonia due to COVID19 disease. Physical exam revealed no abnormal heart sounds, or irregular pulse. Routine 12- lead EKG was performed on admission (Figure 1).
- Past History: She reported having an abnormal EKG in the past with history of palpitations, on beta blocker.
- Family history: There is no history of sudden death in the family. Patient reported a history of congenital heart disease in her daughter.
ECHO showed LVEF of 55-60% with no valve abnormality. Cardiology suggested no intervention was necessary as the incidence of symptomatic Brugada syndrome in a female with no prior history is low. Patient was discharged after the resolution of her presenting symptoms1.
Interestingly, after one week the patient with symptoms of shortness of breath. EKG done at this visit showed the same pattern (Figure 2).
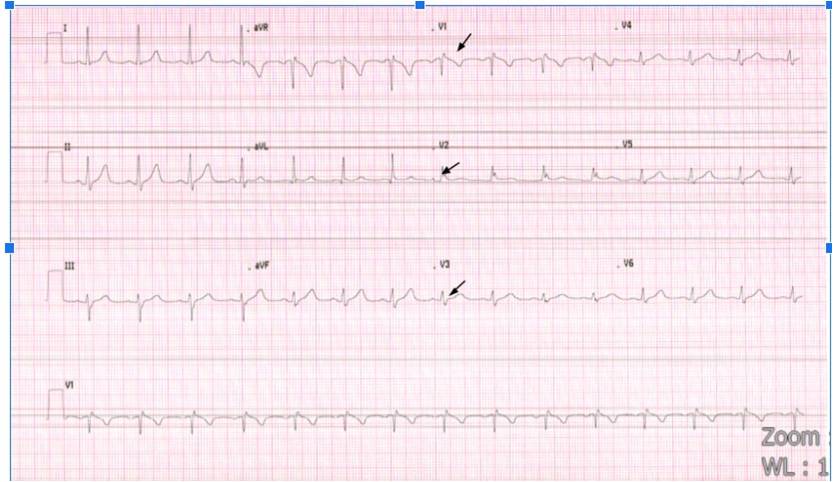 Figure 1: Note the right bundle branch block pattern seen in V1-V3 seen on patient’s EKG obtained at admission in the ER
Figure 1: Note the right bundle branch block pattern seen in V1-V3 seen on patient’s EKG obtained at admission in the ER
 Figure 2: Note the right bundle branch block pattern seen in V1-V3 seen on patient’s repeat EKG obtained a day after admission
Figure 2: Note the right bundle branch block pattern seen in V1-V3 seen on patient’s repeat EKG obtained a day after admission
Discussion:
The 2017 AHA guidelines recommend no treatment for patients with Brugada ECG pattern, who are otherwise asymptomatic due to low incidence of sudden cardiac death or ventricular tachyarrhythmias in patients with Brugada pattern alone as compared to the high morbidity rates associated with ICD implantation or using antiarrhythmic drugs3.
In this case scenario, we followed the patient with repeated EKG and close monitoring on telemetry due to the lack of symptoms like syncope, palpitations, or history of sudden cardiac arrest.
Latest screening guidelines indicate EKG for first degree relatives every two years; who have a history indicative of syncope or ventricular tachyarrhythmia6.
Conclusion:
- This case report highlights a Brugada pattern present in an asymptomatic patient and the need for screening and follow-up on such patients.
- A thorough history and telemetry monitoring including repeat EKG would be beneficial.
- Cardiology follow-up in an outpatient setting would prevent incidence of sudden cardiac arrest.